Migraine can have a debilitating effect on an individual’s performance at work, so it’s vital employers take steps to reduce the triggers for an attack and provide adequate support.
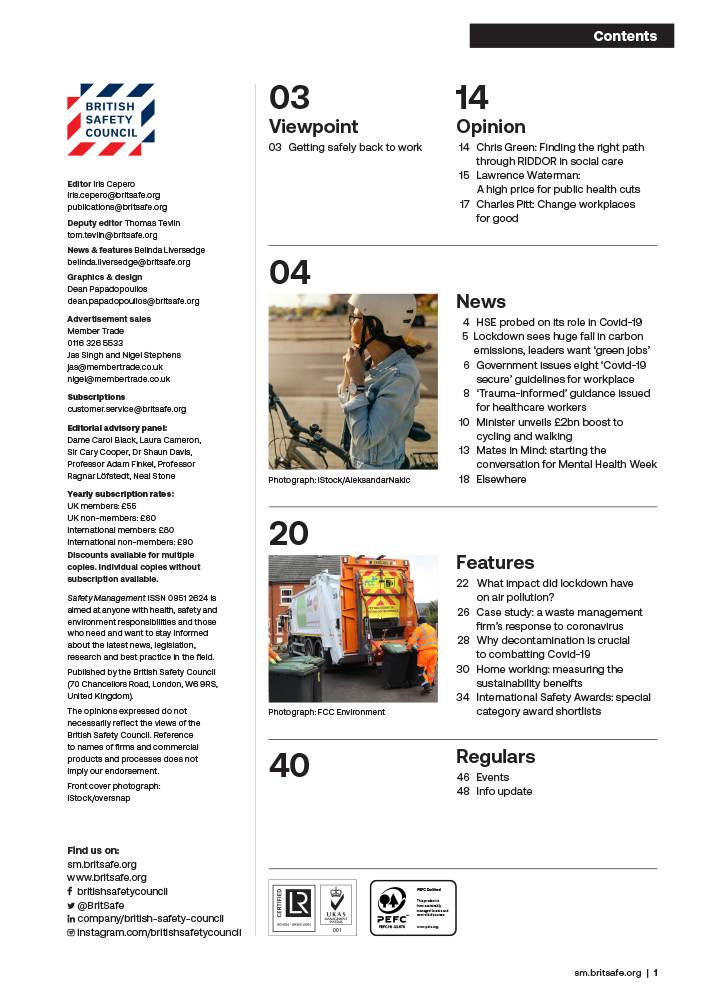
Features
Migraine in the workplace: what needs to change?
What is migraine?
Migraine is a common but complex neurological disorder that can have an enormous impact on individuals, including in their working lives. Affecting one in seven and approximately 10 million people in the UK, it is most common among adults of working age: studies by the Global Burden of Diseases, Injuries, and Risk Factors (GBD) highlighted the Years of Life Lived with Disability through migraine were highest in the group aged 15–49 years.¹
 Photograph: iStock/PeopleImages
Photograph: iStock/PeopleImages
People who live with migraine will experience migraine attacks, which typically involve several distinct phases, outlined below:
In addition to the stages in an attack, there are several different types of migraine, each with a diverse list of symptoms, including:
- migraine with aura – around one in three people with migraine will experience aura, the symptoms of this stage can include visual disturbances such as flashing, coloured or flickering lights or patterns, or even temporary blindness
- hemiplegic migraine – a type of migraine involving weakness on one side of the body
- vestibular migraine – which can include features of vertigo, dizziness or balance problems.
The most common type is migraine without aura, which usually involves each of the stages above apart from aura.
Treatments for migraine
There are various treatments available for migraine. These include acute treatments, which are taken at the onset of an attack to reduce the symptoms, and preventive medications, taken to prevent attacks, or reduce their frequency or severity. The latter tend to be suitable for people experiencing four or more migraine attacks a month.
Acute medications may include over the counter painkillers, triptans (which reduce the pain and sickness of a migraine attack at the time they are taken) and anti-nausea medications.
Recently, several new treatments for migraine – including calcitonin gene-related peptide (CGRP) monoclonal antibodies and gepants – have been developed and approved for use on the NHS. Access to these medications, however, is dependent on a number of factors, including prior failure on other preventive medications.
It is important that people with migraine consult their healthcare professional to find the correct treatment for them. Particularly with preventive medications, it can take between six weeks and three months to fully assess the impact of a treatment, and healthcare professionals may also advise starting on lower doses and gradually building this up in order to help minimise side effects.
Migraine in the workplace
Migraine triggers in the workplace
Migraine triggers are complex, and experiences can be unique to the individual; something that triggers an attack in one person may have no effect on another. Commonly reported triggers of migraine attacks include:
- being hungry or thirsty
- feeling stressed
- changes to one’s usual routine.
With migraine triggers, it is useful to assess whether something is a trigger or is in fact an early warning sign of a migraine attack starting. For example, someone may report that strong smells are a migraine trigger for them, however it may actually be the case that when a migraine attack is beginning, their sensitivity to smells increases, and so they notice scents more than they normally would, leading them to assume the strong smells had triggered an attack.
As physical working environments can differ considerably between sectors and industries, they may present different potential for exposure to triggers. From the harsh fluorescent lighting of supermarkets to the noise of a classroom or glare of computer screens in an office, there are likely to be workplace triggers that are difficult to avoid. Having mechanisms for staff to raise concerns about individual triggers is therefore important.
Workplace stress
Regardless of physical working environment, most people with or without migraine probably have some experience of workplace stress. As discussed, stress is one of the most commonly cited triggers for migraine attacks, with many people noticing stress as a contributing factor in the run-up to an attack. Increased levels of stress can be a trigger in and of itself, but high stress levels can cause a ripple effect into other areas of life – it can have a detrimental effect on sleep, eating habits and general wellbeing, which, in turn, can be potential trigger factors for migraine attacks.
What role do employers have in supporting staff with migraine?
With migraine impacting a significant number of people of working age, it’s crucial that employers are aware of their duties under the relevant legislation, and beyond.
Reasonable adjustments
For some people living with migraine, the condition may meet the definition of disability under the Equality Act 2010 (and the Disability Discrimination Act 1995 in Northern Ireland). This will depend on several factors, including the frequency of migraine attacks and the severity of their impact on the individual.
Despite its prevalence as a condition in the UK, it seems many workplaces fall short when it comes to the support they provide to staff with migraine. More than half (56 per cent) of people who responded to The Migraine Trust’s 2023 workplace experiences survey said their workplace had not made reasonable adjustments to help them manage migraine attacks at work.²
 Credit: The Migraine Trust
Credit: The Migraine Trust
And yet, for many people with migraine, adjustments that are relatively simple and low cost can make a considerable difference, resulting in less absence and better overall workplace experiences.
“I’m very fortunate – all of my managers have been very accommodating when it came to my migraine. When I would tell them ‘I’m having a migraine attack’, they would believe me, every single time,” reports Amelia, who lives with chronic migraine.
Much like the symptoms and triggers of migraine, workplace adjustments for migraine will be specific to an individual. That said, examples of common adjustments include:
- amendments to absence management processes to allow for a certain level of disability-related absence. Since migraine attacks typically last between four to 72 hours, people with migraine are more likely to take short-term sickness absence due to their condition. Employers might therefore look at discounting certain absences relating to migraine so as to avoid triggering absence-management sanctions
- flexible working arrangements, which might allow people with migraine to better manage their workloads during periods of reduced symptoms
- changes to the physical environment, which might include providing appropriate assistive technology or anti-glare screen protectors for staff working on computers
- consideration of working from home – for many people with migraine, the home environment is most easily tailored to their individual needs and for roles where work can be done remotely, this might be a suitable reasonable adjustment to consider.
Good practice
Employers should seek to support employees who advise they experience migraine, regardless of whether the individual is classed as having a disability under the relevant legislation. Creating a culture in which migraine is understood and talked about openly, means that staff will feel more comfortable to share that they have migraine and ask for the support they need.
Additionally, irrespective of whether an employer is aware of a particular member of staff who experiences migraine, and who requires reasonable adjustments to be made, there are many small changes that organisations can make to ensure their workplace is suitable and appealing to people with migraine generally.
Improving the physical working environment
Migraine affects one in seven people, and the likelihood that it will impact current or prospective staff, as well as customers or clients who engage with an organisation, is high. Therefore, adopting good practice, especially when considering the physical workplace, is key to supporting staff retention and wellbeing.
 Andrea Quinn is senior communications officer at The Migraine Trust
Andrea Quinn is senior communications officer at The Migraine Trust
Identifying areas in the physical workplace that could be improved can make a huge difference: installing softer lighting, designating quieter working areas, or reviewing use of fragrance (for example, in cleaning materials) are all ways to reduce some of the potential environmental triggers.
Addressing stress
Addressing the causes of stress at work is a reasonably simple and effective action that both employees and employers can take to help reduce the impact of migraine. Looking at aspects like workloads, systems and processes, and ensuring employees are able to take regular breaks will all be helpful in reducing stress.
The Migraine Trust’s Workplace Pledge
Migraine can have a significant impact on individuals in the workplace. A survey by the Migraine Trust found that:
- 34 per cent of respondents felt discriminated against at work
- 29 per cent said that they had to move from full-time to part-time work, and 33 per cent said they had to leave their job altogether.
The ramifications of migraine go beyond these personal impacts, with employers and the economy affected. For example, it is estimated that each year in the UK 43 million days are lost from work or school because of migraine, and that migraine costs the economy almost £9 billion.³
Despite the high numbers of people of working age living with migraine, and the considerable effects the condition can have within the workplace, migraine remains poorly understood by employers. Our research also revealed that 45 per cent of respondents felt that their managers did not take their migraine seriously.
We want to help employers create a culture where staff living with migraine feel understood and supported in their employment. To do this, we developed The Migraine Trust Workplace Pledge. We’re calling on employers to take our pledge for the one in seven of their employees with migraine. By signing our workplace pledge, and completing our suggested actions, an organisation is demonstrating that it understands migraine can impact working life and is taking the first step to ensuring people with migraine are supported at work.
On signing the pledge, employers will receive fantastic resources and ideas to increase awareness of migraine in their organisation, tips on changes they can make to their workplace and details of upcoming events and ways to get involved.
While it is true that migraine is a complex condition, simple and straightforward adjustments are often all that is needed for a person with migraine to remain in employment. Beyond this, an understanding and supportive approach from an employer can be transformative in shaping the workplace experience of someone with migraine.
Managing migraine at work: tips for employees
With the right support, most people with migraine can usually manage their migraine symptoms effectively in the workplace.
Self-management
Keeping a migraine diary is an excellent way to identify your migraine triggers and potential challenges in the working environment and can be used in conversations with employers about workplace adjustments. It is important to note, however, that identifying and avoiding triggers is not always easy or even possible; migraine is a complex condition, and attacks can be experienced regardless of whether exposure to triggers occurs.
Talking to your employer about migraine
Many people with migraine will understandably feel daunted by the prospect of talking to an employer about migraine, especially because there can be so much stigma and misunderstanding about the condition. However, your employer will be best able to support you if they know how migraine impacts you.
The Migraine Trust’s migraine in the workplace toolkit
This downloadable toolkit contains information on your rights at work, as well as guidance on how to seek support from your employer.
Andrea Quinn is senior communications officer at The Migraine Trust.
For more information, go to:
migrainetrust.org/get-involved/the-migraine-trusts-workplace-pledge/
migrainetrust.org/live-with-migraine/migraineandwork/
- 0808 802 0066
References
- GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology 2018; 17(11): 954–976. ohaw.co/3Rc2ZVT
- Research reveals that over a third of people have experienced discrimination at work because of their migraines. London: The Migraine Trust, July 2023. ohaw.co/MigTrust23
- Migraine at Work: guidance for managers. Lancaster: The Work Foundation, 2019. ohaw.co/MigraineManagers

FEATURES

India’s path to net zero: a work in progress
By Orchie Bandyopadhyay on 08 April 2025
India is implementing a variety of clean energy measures to hit its target of net zero greenhouse gas emissions by 2070, including plans to rapidly scale up the generation of nuclear power. However, climate experts say significant finance will be required from developed countries to phase out coal power, accelerate renewables deployment and expand the national electricity grid.

Too hot to handle: early arrival of heatwaves in India sparks calls for action to protect workers and the public
By Orchie Bandyopadhyay on 08 April 2025
Temperatures in India in February 2025 were the hottest since records began over a century ago, prompting warnings the country needs to urgently step up efforts to protect both workers and the general population from the health risks posed by extreme heat and humidity.

