Migraine can have a detrimental impact on people’s working lives, but employers can significantly reduce the impact through approaches like allowing staff to work flexible hours to cope with the symptoms and providing quiet areas where workers can recover from a migraine attack.
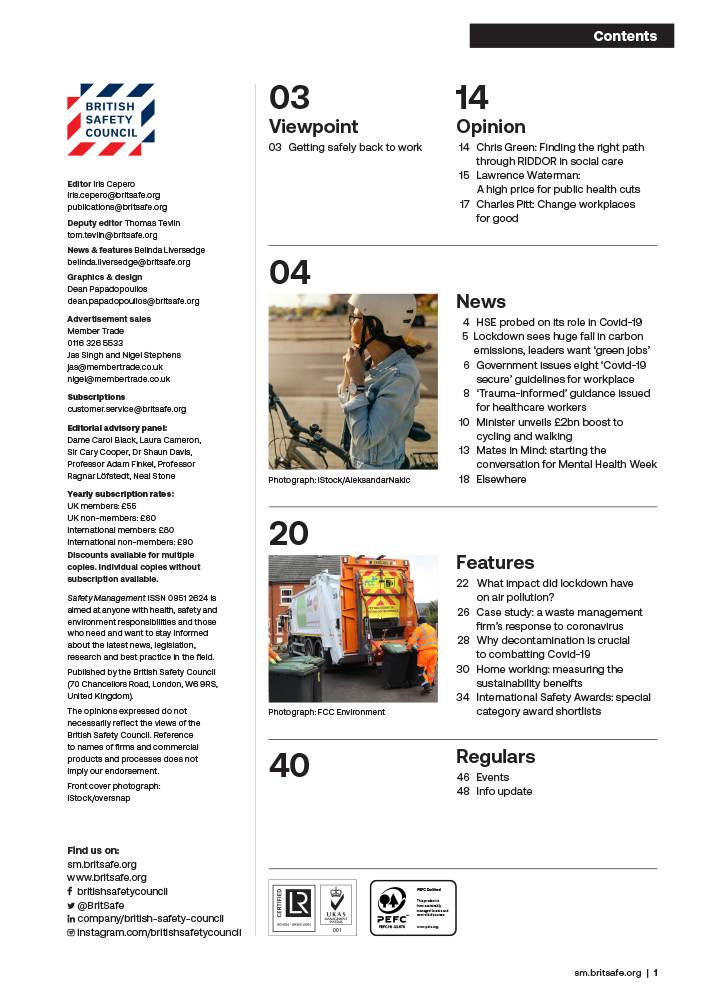
Features
Migraine at work: a real pain
Migraine is a complex neurological condition affecting one in seven people, approximately 10 million individuals in the UK. It is the third most common disease in the world, greater than the number of people living with diabetes, asthma and epilepsy combined. Symptoms of a migraine include head pain, dizziness, nausea and vomiting, visual disturbances, stress and sensitivity to light, sound and smells.
A migraine attack can be incredibly debilitating and leave a person unable to function for many days.

 Migraine can be very isolating because people’s experiences of it can vary widely. Photograph: iStock
Migraine can be very isolating because people’s experiences of it can vary widely. Photograph: iStock
Migraine can be very isolating because people’s experiences of it can vary widely. Some people might have one migraine attack a year, while for others migraine is a chronic condition causing daily pain. Living with an invisible migraine condition can be a lonely experience as no one can see what is happening.
This can create a sense of being misunderstood, but it can feel just as hard to reach out for help. Friends and family can find this equally challenging: they may just see plans getting cancelled or may feel completely hopeless in how to help, which can make the migraine seem like an even bigger problem. Unfortunately, there is no cure for migraine, but there is a range of treatments that can help.
Available treatments for migraine
Usually, effective management of migraine requires a good acute treatment (i.e. acute medicine, such as painkillers and anti-sickness medication) which stops or shortens the attack and provides pain relief. An effective preventive treatment (i.e. preventive medicine, also known as prophylactics, designed to help prevent migraine attacks), may also be needed if the person is experiencing four or more attacks a month.
These preventive medications help reduce the frequency and severity of the migraine. In addition, Botox injections are approved for use on the NHS for the treatment of chronic migraine in adults. Chronic migraine is defined as having at least 15 headache days a month, with at least eight of those featuring migraine symptoms. Calcitonin Gene-Related Peptide (CGRP) monoclonal antibodies (CGRP mAbs) are the first preventive medicines specifically developed for the treatment of migraine. All CGRPs are taken by injection, either monthly or every few months.

 Migraine is a complex neurological condition affecting one in seven people. Photograph: iStock
Migraine is a complex neurological condition affecting one in seven people. Photograph: iStock
It can also be helpful to review any triggers that may be contributing to the attacks, like stress, tiredness, poor or irregular sleep, alcohol consumption, excessive caffeine, not eating regularly and skipping meals.
If a person with migraine has not had a medication review for some time it may be worth them speaking to their GP as there are many more new medications being licensed these days. If the GP feels they can’t offer any further options they may be able to refer the patient to a headache specialist or neurologist. A specialist should review the impact of the person’s migraine, their symptoms and the treatments they have already tried and suggest other treatments that may help. There are different treatments available depending on the individual’s situation.
Some people find dietary supplements helpful for treating the symptoms and severity of migraine, such as riboflavin (B2) 400mg a day, magnesium 400mg a day or co-enzyme Q10 150mg a day. It can take around 6–8 weeks to see a benefit and three months to see the full impact of these.
Some people choose to take all three supplements together or try each one individually – it’s often down to personal preference. Some migraine sufferers also report that acupuncture can be helpful for preventing and treating the symptoms of migraine.
There are some devices that can be useful, such as the Cefaly device, where an adhesive electrode is placed on the forehead and the Cefaly connects to the electrode to produce precise micro-pulses on the upper branch of the trigeminal nerve to treat migraine. However, while the device has been shown to be of benefit to some sufferers, it does not work for everyone. More information about the Cefaly device and user testimonials can be found on the manufacturer’s website.

 Steph Weatherley: "There are a number of reasonable adjustments for migraine sufferers that can make a huge difference at little cost to the employer."
Steph Weatherley: "There are a number of reasonable adjustments for migraine sufferers that can make a huge difference at little cost to the employer."
Migraine triggers at work
Working with migraine can be very challenging. It is estimated that 43 million days are lost from education and work due to migraine in the UK every year. This equates to migraines costing the UK economy an estimated £9.2 billion, over 98 per cent of which comes from lost productivity.
Many aspects of the workplace can contribute to migraine attacks, including artificial lighting, lack of regular breaks, screen time, stress and working long hours. People with migraine may need to take additional sick leave due to the condition; however, many will continue to work and battle through a migraine due to fear of being seen as unreliable.
A recent survey by The Migraine Trust found that 43 per cent of people with migraine felt they weren’t believed when taking time off sick due to migraine, while 32 per cent said they didn’t feel comfortable telling HR about their migraine. Unfortunately, in some cases, people are dismissed from work or feel they must resign, retire or switch to part-time work due to their migraine.
In response to The Migraine Trust’s survey, 43 per cent of people with migraine said they had been financially impacted by migraine’s effects on their career.
Migraine may cause health and safety issues at work, and this can create risks and dangers during jobs where machinery is operated, regular driving is required or where people work in hazardous locations like construction sites, for instance.
If a person with migraine experiences a migraine attack, depending on their symptoms, this may impact their ability to do their job correctly and safely, and in turn this could put the safety of others nearby at risk, such as co-workers or the public. The health and safety risk at work is perhaps greatest for migraine sufferers who experience symptoms of vision disturbance, numbness or weakness in the limbs. However, many people with migraine are aware of their premonitory symptoms that occur prior to the aura or main attack stage, and therefore can usually minimise the risk by safely and immediately stopping work.
In these situations, it is therefore important for the employer to understand the stages and symptoms of a migraine and the reasonable adjustments an employee may need to enable them to stop work in the event of migraine symptoms that could endanger their own health and safety and the safety of others.
Practical support for people with migraine
People with migraine can be supported in the workplace by taking some very simple, yet impactful steps. For an employer it’s crucial to ensure employees feel comfortable talking to their employer, managers and HR teams about their migraine without fear of being dismissed from their job – for example, if they need to stop work for short periods or take short-term sickness absence due to the condition.

 Chronic migraine is defined as having at least 15 headache days a month, with at least eight of those featuring migraine symptoms. Photograph: iStock
Chronic migraine is defined as having at least 15 headache days a month, with at least eight of those featuring migraine symptoms. Photograph: iStock
There are also a number of reasonable adjustments that can make a huge difference at little cost to the employer, including:
- Flexible working
- Time off for medical appointments
- Changes to lighting
- Flexible breaks
- Technology changes – for example, anti-glare computer screens
- Allowing people to work from home if possible – this can make it easier to manage migraine
- Changes to desk and workstation setups – such as positioning office desks to avoid window glare
- Access to drinking water
- Access to a quiet room – so people can sleep or lie down during a migraine, where possible.
For the colleagues of those experiencing migraine, acknowledging a person’s migraine and being supportive can be very reassuring and help the person to be honest about how they are feeling and the impact it is having on them. The sufferer may benefit from having someone to talk to, provide them with a drink to help them stay hydrated during a migraine, or cover their work for a short period while they take a break.
The lack of understanding and stigma around migraine can be very challenging for people with migraine, and it is all too often dismissed as ‘just a headache’. Therefore, employers should educate their employees about what migraine is and how it affects people, as this will make a significant difference to the way migraine sufferers are able to cope with the condition at work and gain understanding, help and support from their managers and colleagues. For more information for employers and migraine sufferers on ways of managing migraine at work, see the Migraine Trust’s Migraine in the Workplace Toolkit.
Conclusion
Overall, migraine is a complicated condition which can be difficult to treat, but there are treatment options that a worker can discuss with their GP.
It can be helpful for an employer and other employees to be aware of migraine and the impact it has, the adjustments that can be made and the support that can be given to help those struggling with migraine in the workplace.
For employers interested in learning more about managing migraine in the workplace, the Migraine Trust offers a range of workplace presentations. For further information on these please email [email protected]
The Migraine Trust helpline offers free, confidential information and support for anyone affected by migraine. The helpline is open Monday–Friday, 10am–4pm (excluding Bank Holidays) on T. 0808 802 0066. There is also a Live Chat and email support and information service, and online guidance. See: migrainetrust.org
Steph Weatherley is senior support services advisor at The Migraine Trust

FEATURES
Why changes to recycling legislation in England are an opportunity, not a burden
By on 12 November 2024

Road safety in India: could better road safety, vehicle technology and enforcement make driving for work safer?
By Orchie Bandyopadhyay on 10 November 2024
India has a poor road safety record, and research shows that commercial vehicles are a major contributor to the problem, with trucks estimated to be the single largest vehicle type involved in impacts leading to fatalities. We look at solutions that could make driving for work and the roads in general safer – from in-vehicle technology that warns truck drivers about unsafe behaviour to improving the design features of major highways.

