Inventors are dragging health screening into the 21st century. But should we be excited or worried about these powerful health intelligence tools?
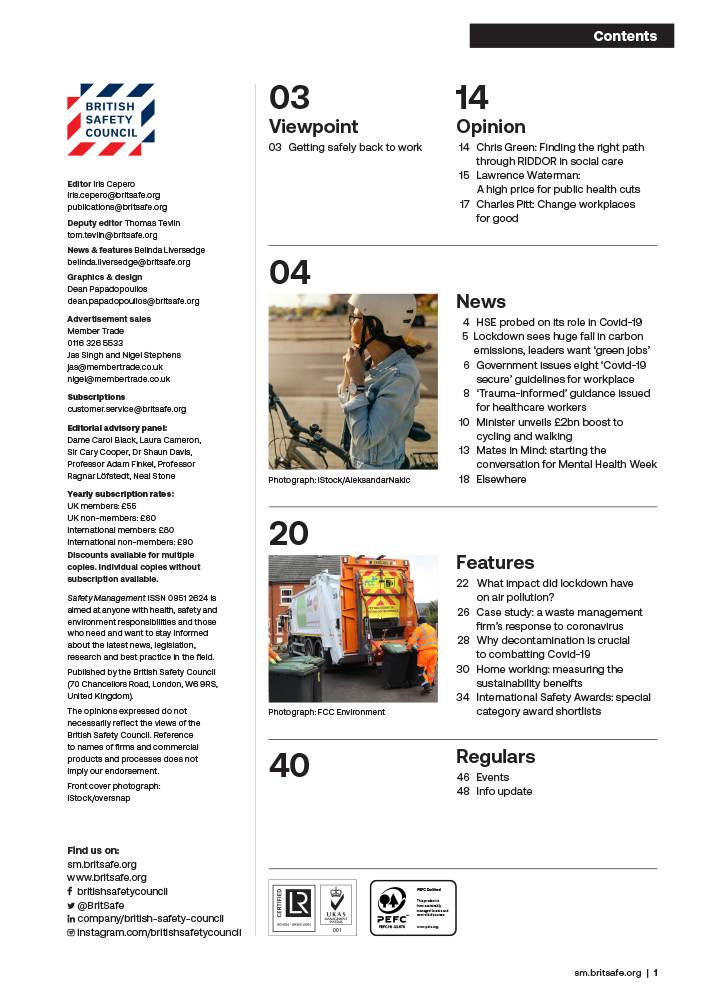
Features
In the blood
We are living in an age of technological revolution. This includes in the field of health. Businesses, it seems, are vying for our blood, our saliva and our DNA. In return, they give us a full analysis of our health risks, disease profile, and the steps we can take to extend life. But would you find out the ‘secrets of your body’, as one poster on the London Underground put it, at the prick of a needle? Or advise your employees to?
At April’s Watercooler conference, one of the many ‘watercooler moments’, was hearing John Godfrey, Chair of the business-led coalition group, Business for Health, say that employers should be ‘bracing themselves’ for this new wave of health intelligence: “We will be able to diagnose cancer much earlier using technology. Employers are going to have to have a big voice in that. It will be a conversation between the employer and their employees about how they are going to use it.”
 Technologies now available are vastly more powerful, can assess for a far wider range of illnesses and disease. Photograph: iStock
Technologies now available are vastly more powerful, can assess for a far wider range of illnesses and disease. Photograph: iStock
Vastly more powerful tools
So, what is health intelligence and should employers be using it? In the first place, health checks and screening at work are not new. However, the technologies now available are vastly more powerful, can assess for a far wider range of illnesses and disease (as well as fitness), and can alert us to predispositions to a particular disease. The need for health checks may not be new, but the technology and its implications are.
It is an expanding and rapidly evolving field, including telemedicine, wearable technologies and augmented and virtual reality. At their most basic, these health intelligent technologies bring health data together – such as age, family history and lifestyle choices around diet and smoking – to build a picture of someone’s health.
At the more sophisticated level it deploys software that can draw on diagnostic information, use real-time data from wearable devices to spot early signs of disease, and allow users to plan health pathways to manage conditions and make medicine more personalised and precise.
NHS – not a preventative service
Cancer will affect one in two of us. Yet, even though we know early diagnosis and treatment leads to much better health outcomes, under a stretched NHS it can be hard to get screened for cancer, even if you have hereditary risk factors.
In the UK, 37 per cent of cancers are diagnosed in A&E and 40 per cent of premature deaths by cardiovascular disease, diabetes, cancer and lung disease are preventable. “We are living in an age of dangerously delayed diagnosis,” says Alex Templeton, founder and CEO of digital health screening platform, Qured. “We test for what we can afford, rather than according to clinical best practice.”
 Alex Templeton, CEO and founder of Qured speaking at the Watercooler conference in London
Alex Templeton, CEO and founder of Qured speaking at the Watercooler conference in London
With the NHS under ever-increasing pressure, jobs like referral and early intervention will become the work of others in society. We’ve seen this recently with pharmacists given the power to refer customers to specialists for symptoms such as lumps. Now employers will have to step up too, says Sir Cary Cooper, Professor of Organizational Psychology and Health at Manchester Business School: “The NHS is not able to do its job. It’s teetering on being an emergency service but not a preventative one. Therefore, we’re going to see more provision to employers of both physical and emotional indicators to help them [look after their workers].”
In March, the government appointed someone to specifically get this work started. Professor John Deanfield CBE, the government champion for personalised prevention, will explore how businesses could be incentivised to support disease prevention outside of the NHS. Work will show how we can “predict and manage disease more effectively using personalised data.”
Professor Cooper says it’s positive that health testing is being made more widely available to people and businesses via more accessible health intelligence tools: “The majority of people in the private sector are employed by SMEs not by the big companies and they have to find a cost-effective way of [health provision]. These technologies [are] probably the beginning of that process.”
 Professor Cary Cooper: "“The NHS is not able to do its job. It’s teetering on being an emergency service but not a preventative one."
Professor Cary Cooper: "“The NHS is not able to do its job. It’s teetering on being an emergency service but not a preventative one."
‘Productivity depends on health’
The other real big driver for health intelligence is productivity. In the UK last year, workers took a record number of days off due to sickness, with long-term sickness also reaching record highs, said the ONS. In parallel, the UK saw zero annual growth in economic output per hour worked in the final quarter of 2022.
Alex Fairweather, Strategic Development Manager at Randox Health, says these are all reasons for health assessments to grow in demand: “There’s a growing awareness among companies that the health of the nation is not in a great state – how that’s affecting companies in terms of their output is I think of primary concern.
“Productivity, what they’re getting out of the profitability of the company, does depend on the health of the employees and wellbeing, not just purely from an individual output point of view but in terms of retaining those people.”
New solutions
This is where health intelligence, like Qured, which offers a way to plan and carry out health assessments and screening via one app, claims to offer a solution. It works by taking a person’s clinical data, family medical history and personal risk factors to build a personalised health plan. This could include screening for lung, breast, bowel or testicular cancer and other diseases.
Blood testing can give a softer, less daunting entry point into understanding how to build better general health such as nutrition and hormone health. Crucially, it cuts out waiting times and users don’t even have to leave home. Its blood test can be done from the sofa, as new technology uses microneedles thinner than an eyelash.
 Qured's at home blood testing kits use microneedles thinner than an eyelash. Photograph: Qured
Qured's at home blood testing kits use microneedles thinner than an eyelash. Photograph: Qured
Problems
Health screening and assessment might sound like a ‘win-win’ then for individuals and businesses alike. However, it’s a complex area. False positives in screening for cancer is an issue.
The UK National Screening Committee, which sets things like the age limit for testing for cancer and advises ministers and the NHS on decisions around screening, says “no screening test is perfect and there will always be some incorrect results.” A false result can cause ‘anxiety or false reassurance’, lead to unnecessary treatment or life decisions.
Alex Templeton says that Qured follows the international gold standards for testing and that it’s ahead of the game. For example, the government has set a new target to test people for bowel cancer from aged 50, but although the NHS is moving towards this, it’s still currently only available for people aged 60+. “The move by the NHS to offer it to younger people over time only serves to highlight the efficacy of broader screening and how much more needs to be done,” he says. “Late detection is the main reason why our survival rates lag those of other developed economies across most common cancers.”
He adds the tests that Qured uses as ‘testing pillars’ are those for which early intervention can make a big difference. “You can intervene and drive a better health outcome for that person. And in those kinds of contexts it’s always better to know. Because early intervention is key and knowledge is power when it comes to our health.”
Data danger?
There are also data privacy concerns. Could health information be used against a worker? Under data protection laws, an employer cannot access an employee’s full health records and when it comes to health apps drawing in data, the employer will only receive information when a certain threshold of users has been reached. The argument goes, that, much like with an employee assistance programme, a service can track health trends and risks across the business, but nothing that can identify an individual.
 Smartphone technology can now help manage diseases, like this woman with diabetes who swipes for her glucose levels. Photograph: iStock/AzmanJaka
Smartphone technology can now help manage diseases, like this woman with diabetes who swipes for her glucose levels. Photograph: iStock/AzmanJaka
But the concern remains, says Professor Cooper. An individual will still be encouraged to discuss their diagnosis when seeking support and there needs to be trust at that point: “The test itself could be risky, what happens if you find out you’ve got something? Is [the diagnosis] a vehicle to let them go? ‘I’m sorry you are officially ill, you’re going to have to get treatment and we don’t have the back up’, or they lose their jobs.”
Employers need policies to support the long term sick and a plan for proper care: “How are you going to help them to get back to work after they’ve been treated? It might look good [to offer health screening] but when they find out things, what’s the strategy to deal with it?”
Communicating results
Communication and guidance for onward support need to be prioritised, agrees Marcus Herbert, British Safety Council’s head of wellbeing. “If an organisation is looking to partner with a health assessment provider or a health screening provider, they should be definitely discussing not just what tasks are included, but who is actually delivering this information, what is their qualification or background and what do you do from a governance perspective to ensure the quality of delivery?”
Marcus, who has delivered thousands of health assessments when working at Nuffield Health as a physiologist, knows too well how even qualified professionals can slip up. He recalls how one man was really stressed and worried about his blood test results, which he was told showed he was at “immediate risk” of prostate cancer.
It turned out this was not the case. It was merely because he was a cyclist and cycling is known to increase inflammation of the prostate and the Prostate-Specific Antigen levels in blood. A urologist saw him and cleared up the mistake that the doctor – a locum who was not used by the company again – had made when giving the test results. “It’s just evidence that it can happen,” says Marcus. “You can deliver the same information in two different ways, the right way and the wrong way, and that can determine the experience for the end user.”
The verdict
Health intelligence is a complicated issue. Who pays for the treatment once a test has identified it is needed and what policies are in place to support people to stay in or return to work are all big questions to solve before even beginning to seriously consider promoting health intelligence to your staff.
 A third of Gen Zers trust TikTok more than doctors, a US survey by CharityRx recently found. Photograph: iStock
A third of Gen Zers trust TikTok more than doctors, a US survey by CharityRx recently found. Photograph: iStock
There’s also our squeamishness around finding out problems. “It’s a real feature of the human condition that sometimes we prefer not to know things that we ought. We think ‘we’re ok, it won’t happen to me,’” admits Alex Templeton. “Sadly that’s not the case. And, in life, generally we know that when you have a plan you get a better outcome than just winging it, whereas most people in this country do wing it with their health.”
Culture shift
But we know that things are changing culturally. A third of Gen Zers trust TikTok more than doctors, a US survey by CharityRx recently found. Young people are fully comfortable with using technology and their phones for research and seeking treatment.
Health assessments are also becoming less the preserve of the 1 per cent and something all workers will be demanding. “A lot of the [older] generation of leaders seem to think that it’s the responsibility of an individual to look after their health – they turn up for work and they need to do what they do,” says Alex Fairweather.
“I think that’s shifting, the younger generation are now turning into managers and leaders within businesses – they realise a company has to support an individual to be healthy at work and help their productivity. So I think it’s a bit of a culture shift and mindset shift.”
Discussing our fallibilities shouldn’t be a big deal anymore: “It’s not just as simple as ‘we should provide health assessments for our employees to make sure they’re well and to look after them if they’re unwell’, it’s what we do to get them even healthier, to stop them becoming ill and help retain them in the business.”

FEATURES
Why changes to recycling legislation in England are an opportunity, not a burden
By on 12 November 2024

Road safety in India: could better road safety, vehicle technology and enforcement make driving for work safer?
By Orchie Bandyopadhyay on 10 November 2024
India has a poor road safety record, and research shows that commercial vehicles are a major contributor to the problem, with trucks estimated to be the single largest vehicle type involved in impacts leading to fatalities. We look at solutions that could make driving for work and the roads in general safer – from in-vehicle technology that warns truck drivers about unsafe behaviour to improving the design features of major highways.

